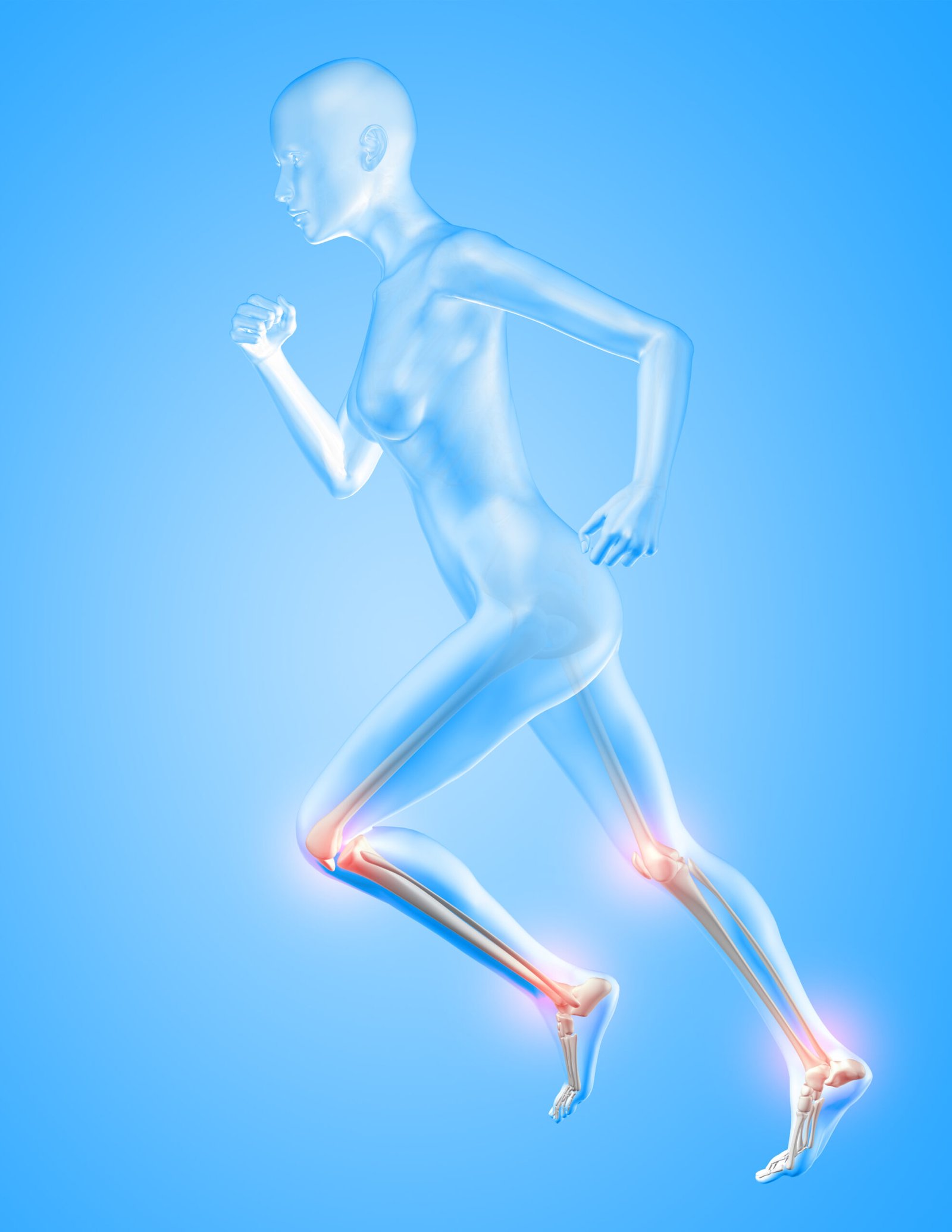
Proper exposure is crucial for the accurate placement of the artificial joint (prosthesis) and ensures that the surgeon can perform the necessary procedures with precision.
- Soft Tissue Dissection :- After making the initial incision, the surgeon carefully dissects through the layers of soft tissue, such as muscles and tendons, to expose the joint. The goal is to minimize trauma to surrounding tissues while providing adequate access.
- Retraction :- Specialized instruments, such as retractors, are used to gently move aside muscles and other structures, providing a clear view of the joint. This step is crucial for the proper placement of the prosthesis.
- Capsular Incision :- In some cases, the joint capsule, a tough, fibrous structure surrounding the joint, may need to be incised to expose the joint space. This allows the surgeon to remove the damaged or diseased joint surfaces and prepare the area for the artificial joint.
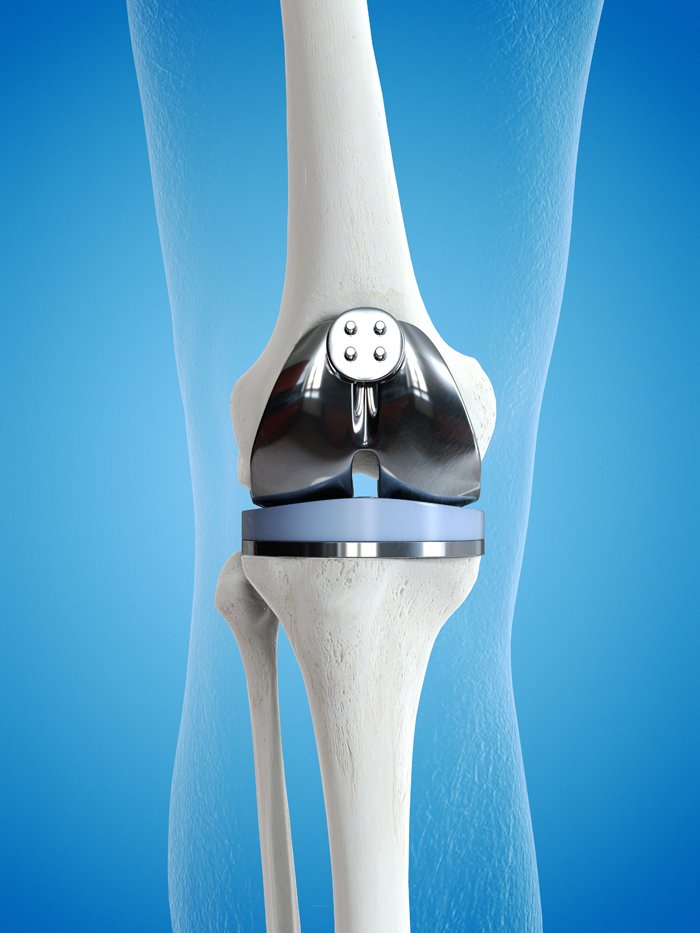
- Bone Preparation :- Once the joint is adequately exposed, the surgeon prepares the bone surfaces to receive the artificial joint components. This may involve removing damaged cartilage and bone, shaping the bone to fit the prosthesis, and ensuring proper alignment.
- Implant Placement :- The artificial joint components are then carefully inserted and secured into the prepared bone surfaces. The type of implant and the method of fixation (cemented or uncemented) depend on various factors, including the patient’s age, bone quality, and the surgeon’s preference.
- Closure :- After the joint replacement components are in place, the surgeon closes the incision, often using sutures or staples, and may apply dressings to the wound.
The exposure of the joint is a critical aspect of joint replacement surgery, and the surgeon’s skill and experience play a significant role in achieving optimal outcomes.